Pain and other chronic symptoms—like IBS, vertigo, tinnitus or bladder issues—can take over our lives. Physical symptoms naturally create fear, and symptoms and fear together can become the center of our attention, pushing everything else into the background.
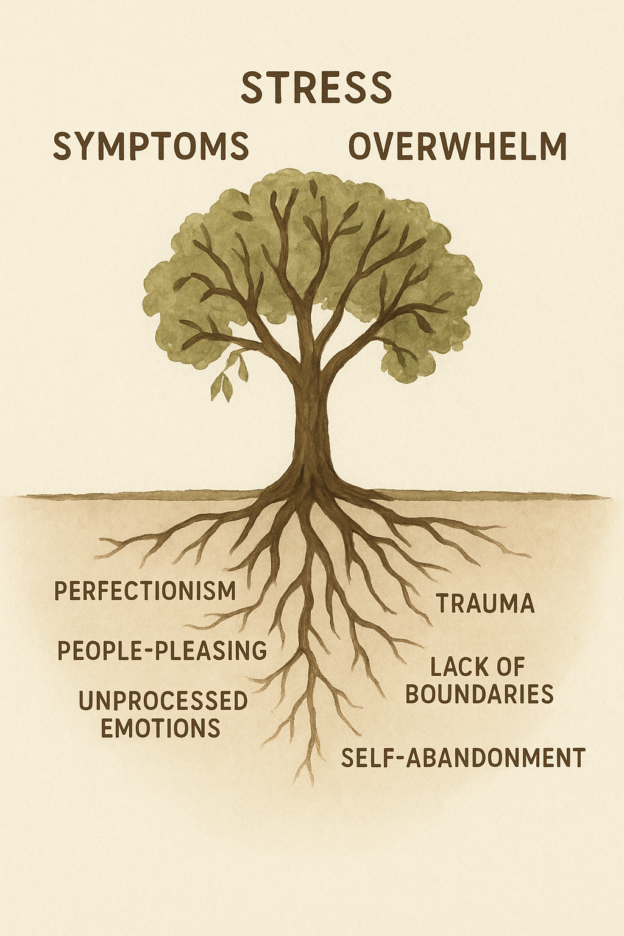
When pain or symptom keep us from doing the things we enjoy, it’s common to feel anxious or depressed. In fact, most people who struggle with chronic pain also experience anxiety or depression. It’s not always clear which came first, because they are closely connected. Many people with chronic symptoms have experienced childhood adversity, and are likely to be perfectionists or people-pleasers—traits that can increase stress and make us more vulnerable to both physical and emotional symptoms.
While chronic pain and other physical symptoms appear to be based in the body, research shows that trauma, emotions and stress play a powerful role—even sometimes when pain seems to have a clear physical cause.
I experienced this firsthand. Years ago, I developed chronic wrist tendinitis that was attributed to typing too much. My pain was real and constant, and I tried everything—chiropractic, physical therapy, massage, acupuncture, Alexander Technique, and Feldenkrais classes. Nothing helped for long. I had to stop doing many things I loved. I wore wrist splints, used voice-recognition software, and avoided cooking, gardening, and knitting. Despite all these precautions, I was in pain for more than two years.
Then I found Dr. John Sarno’s book Healing Back Pain. He discovered that many people who had physical findings that might cause pain—like herniated discs or arthritis—had completely different pain experiences. Some had severe pain, while others with the same imaging results felt none at all. One large study of over 3,000 people found that spine changes seen on MRIs are usually a normal part of aging and don’t necessarily cause pain. His work with his patients demonstrated that emotional stress and repressed anger can create very real physical pain. He helped many thousands of people recover from chronic pain with his medical practice and his books. I was one of them.
It’s important to note that pain or other symptoms are not “all in your head.” Chronic symptoms are absolutely real. But all our experiences are mediated by the brain, and our brains interpret pain based on not only sensations sent from the body, but also based on expectation, and the perception of danger. If we’re afraid that something is wrong with our bodies, or of conflict, negative emotions, or anything else we experience, pain and other symptoms can begin or intensify. On the other hand, if we feel safe and confident in our body’s strength, and in our ability to handle our emotions and our relationships, they can fade—even when nothing physical has changed. This is why treatments that reduce fear and increase a sense of safety can be so effective. The fact that changes in in how we interpret the world impact our symptoms is why we call these symptoms “neuroplastic.”
Over the past several years, there has been increasing evidence supporting Dr. Sarno’s theory, and new treatments have begun to be proven to help patients overcome neuroplastic symptoms. In 2020, I completed training with the Pain Psychology Center to work with clients using Pain Reprocessing Therapy (PRT). A study at the University of Colorado found that people with long-term back pain experienced major or complete recovery after just four weeks of PRT.
PRT helps retrain the brain to interpret pain signals differently. It uses mindfulness, cognitive, and behavioral techniques to reduce fear, calm the nervous system, and build a sense of safety in the body. As fear decreases, pain often does too—sometimes permanently.
Chronic symptoms, as miserable as they can be, often serve hidden purposes. They may give us permission to slow down, rest, or seek care from others. They may distract us from emotions we’d rather not face. Understanding these patterns can help us reclaim our energy and our lives.
When we start to truly trust that our bodies are strong and resilient, and that we can handle our emotions and the stresses in our lives, we can stop letting pain dictate our choices. With the right tools and mindset, recovery is possible—and life can feel full and joyful again.
Take a test to see if your chronic pain or symptoms are likely treatable using a mind-body approach
References:
- Sarno, M.D., John E. Healing Back Pain: The Mind-Body Connection. New York, NY: Warner Books, 1991.
- Sarno, M.D., John E. The Mindbody Prescription: Healing the Body, Healing the Pain. New York, NY: Warner Books, 1998.
-
Published online 2014 Nov 27. doi: 10.3174/ajnr.A4173